Fascia Iliaca Compartment Block
Rationale.
WHY FICB?
Fractured neck of femur (NOF) is a common presentation in the emergency department. (1) Achieving adequate analgesia can be challenging. Regional anaesthesia has the potential to provide fast, direct and prolonged analgesia with fewer systemic side effects compared to procedural sedation or systemic analgesia. (2) In advanced-age patients with multiple comorbidities, managing fractures by blocking nerve branches for analgesia can significantly reduce the need for opioid use. (3, 4, 5)
Unsurprisingly, RCEM has set the Fascia Iliaca Compartment Block (FICB) as the standard pain management strategy for patients with a NOF. (6) Consequently, in this section, we focus on FICB, although ultrasound-guided femoral nerve block is also a good alternative to achieve a similar purpose.
WHY USE ULTRASOUND-GUIDED NERVE BLOCKS?
The original technique developed by Dalens was centred on anatomical landmarks; however, more physicians are using ultrasound as an aid for this block. With reason, as ultrasound-guided FICB has shown to have greater efficacy and safety. Ultrasound guidance allows clinicians to visualize the target structures (nerve and fascial planes), monitoring the advancement of the needle and surrounding structures in real life to guide accurate placement of the anaesthetic agent adjacent to the nerve.
WHO?
As stated above, the primary group would be patients presenting with a proximal femur fracture; however, also patients with patella fractures or patella/quadriceps tendon injury can also benefit from a FICB.
Anatomy.
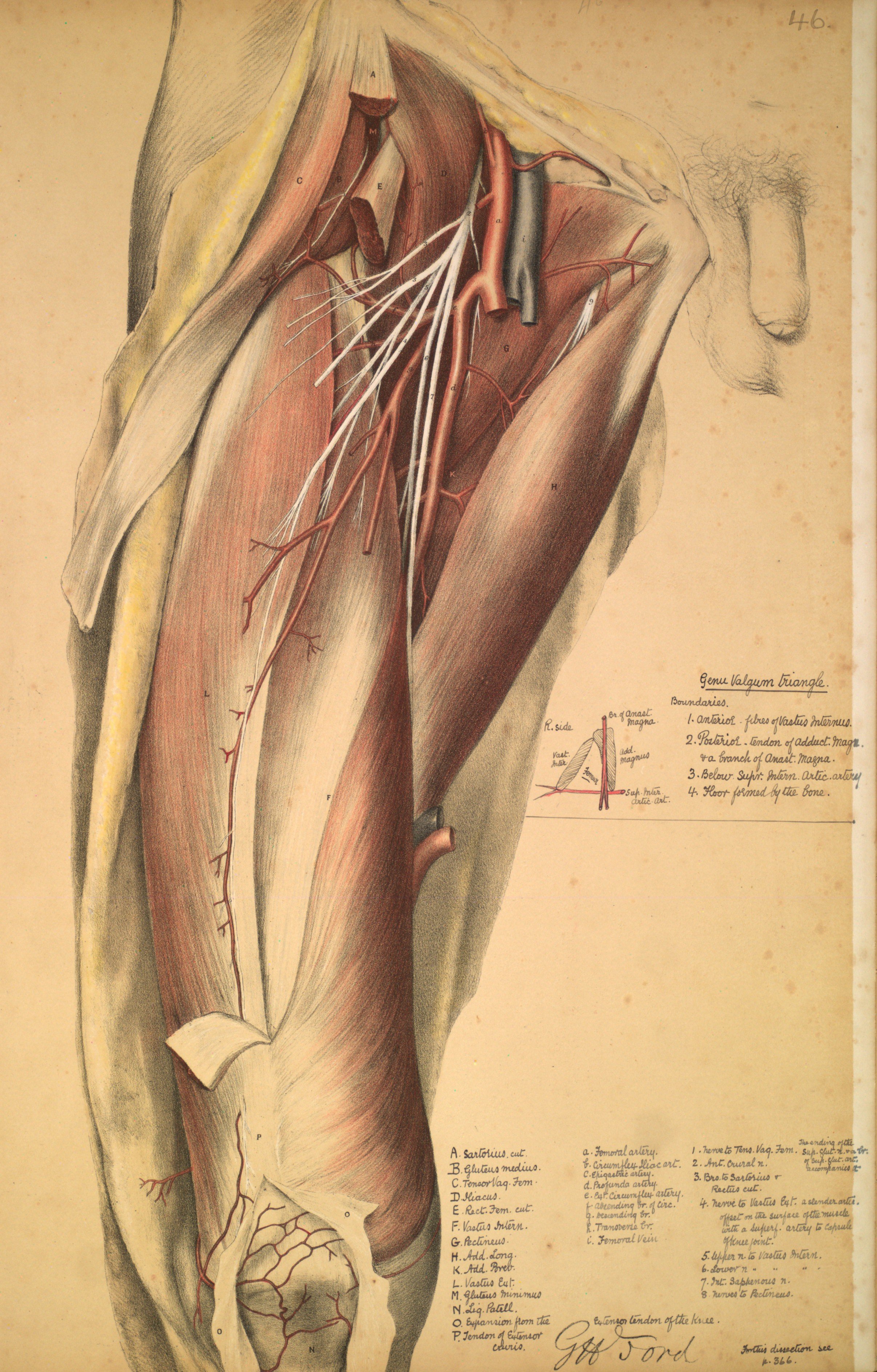
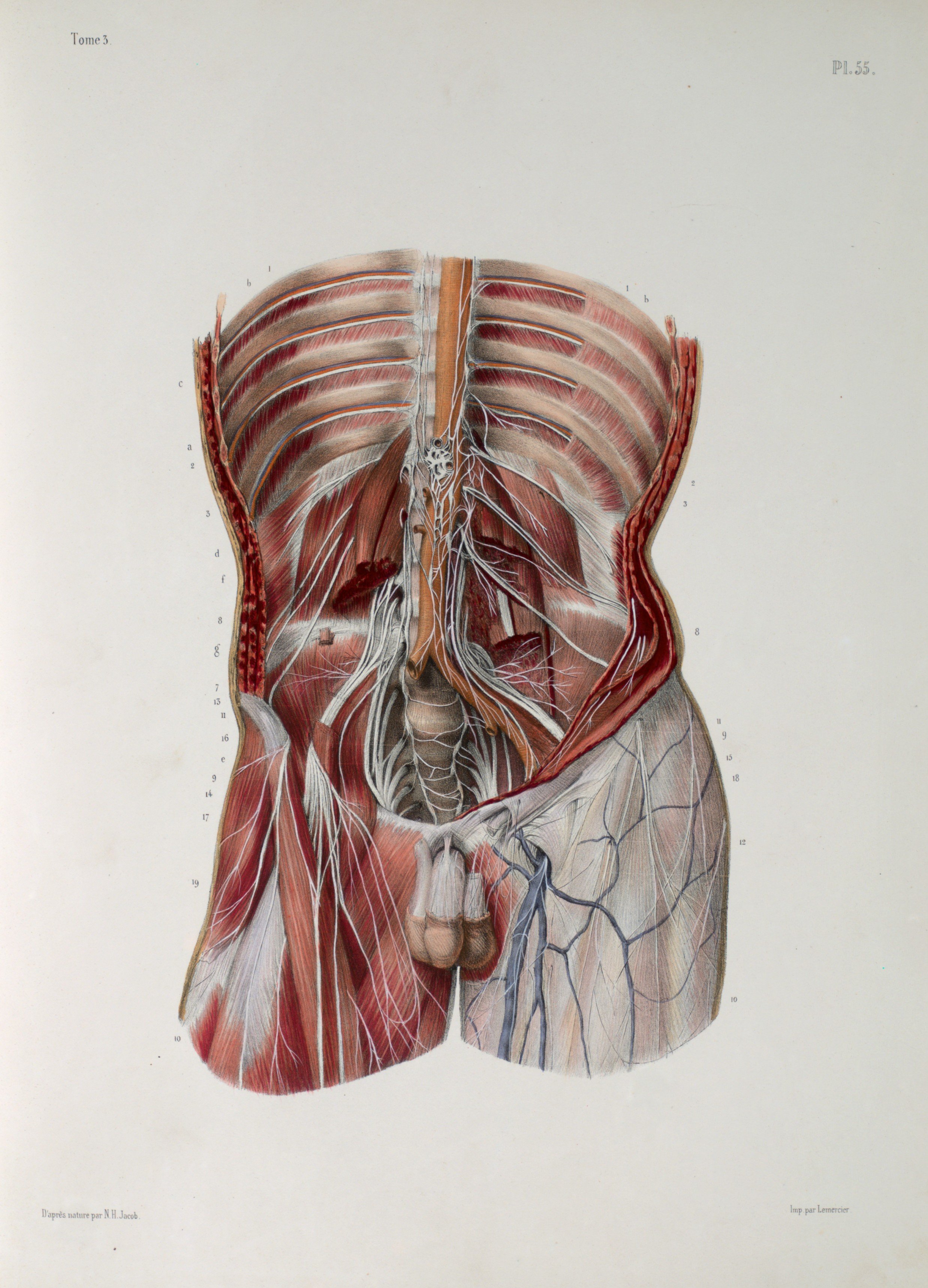
Three major nerves are responsible for the hip innervation: the femoral, the obturator and the lateral femoral cutaneous nerve.
The femoral nerve is the largest, arises from L2-L4 before descending over the iliopsoas muscle. More caudally it sits laterally to the femoral artery and vein. It should always be blocked after placing a FICB.
The lateral femoral cutaneous nerve originates from L2-L3. It runs via the lateral border of the psoas major muscle over the anterior aspect of the iliacus muscle, towards the anterior spinia iliaca. The LFCN gets blocked in about 80-100% of the procedures.
The obturator nerve originates at the L2-4 ventral rami but descends more medially, in the psoas muscle, where it runs behind the common iliac artery. Because of this location it is variably blocked by the FICB.
The fascia iliaca lays, as the name suggests, on top of the iliacus muscle. It runs from the iliac crest medially where it merges with the fascia of the psoas muscle. The ilio-psoas muscle itself runs further under the inguinal ligament towards the anteriomedial aspect of the hip. The sartorius muscle crosses over from the anterior superior iliac spine (ASIS) to the medial upper leg and is used as a reference.
The inguinal crease contains, from medial to lateral, the femoral vein & artery and the femoral nerve. Depending on the approach you use you will see the above mentioned structures (see images at procedure).
Considerations.
Absolute contra-indication is an allergy to local anaesthetics. Relative contra-indications are anticoagulant use, severe thrombocytopenia and coagulopathy.
As with every invasive procedure, there is a risk of infection and bleeding post-procedure. Further, the block might fail, or local trauma to closely associated structures can be caused. Lastly, although the use of ultrasound increases safety in this procedure, local anaesthetic systemic toxicity is a rare but well-known complication of regional anaesthesia.
The RCEM has recently alerted on a ‘side-effect’ of an effective block: by removal of the stimulus, patients that previously received opioids might become more prone to respiratory depression and sedation.
For this reason, this procedure should be done under monitoring in a sterile environment. The patient should be informed of the procedure, the alternatives and possible complications, and at least verbal consent should be obtained.
A fascia iliaca block is a volume block, i.e. the success depends on the spread of 30-40ml of anaesthetics. Depending on your patient’s weight, you might want to dilute the local anaesthetic chosen.
Procedure.
SETTING
Because of the possible complications, the procedure should take place in the resuscitation area where the patient can be monitored before, during and at least 30 min after the procedure. It should be performed by a trained clinician, and emergency drugs, including intralipid solution (for management of systemic anaesthetic toxicity) , should be readily available.
There are two approaches: infra-inguinal and supra-inguinal. The same equipment is needed for either approach. The first technique appears to be less technically challenging, but potentially the supra-inguinal approach provides a better reach of the lumbar plexus and lateral cutaneous/obturator nerve blockage. (8, 9)
EQUIPMENT
• Bedside monitor
• High frequency linear ultrasound probe
• Sterile gloves
• Antiseptic solution
• Local anaesthetic of choice (dose calculated and checked)
• Sterile peripheral-nerve block pack:
• Sterile US probe sleeve and sterile gel
• 2x 20 mls syringe to draw up local anaesthetic.
• Syringe extension to connect syringe to nerve block needle
• 20-22G Nerve Block needle (or spinal needle)
• Adhesive dressing
INFRA-INGUINAL APPROACH
Put the patient prone, make sure you have a comfortable working position and you have the ultrasound screen in direct sight (usually on the contralateral side of the patient).
Select the high frequency linear probe and select ‘musculoskeletal’ in presetings. !Don’t forget to put (non-sterile) jelly on probe already!
Clean the skin with an antiseptic, let it dry by air.
Clean your hands and put on sterile gloves.
Set up sterile field at level of inguinal crease.
Set up sterile sleeve onto probe and put sterile gel on. The probe marker should point to the patient’s right.
Visualize the femoral artery. Lateral and deeper you will see an hypoechoic structure, which is the iliopsoas muscle. In between those structures lies the hyperechoic femoral nerve.
Move your probe laterally until you visualize the sartorius muscle in the edge of the screen. You can see the bright hyperechoic fascia running under this and over the iliopsoas muscle. This is the area you are aiming for.
Place a 1-2ml skin wheal of local anaesthetic next to the probe at the desired needle entry point
Advance your needle while visualizing it in plane. You might feel a ‘pop’ when you pass through the fascia.
After a negative aspiration, inject 1-2ml to confirm the right position.
The anaesthetic should separate the fascia in both the medial as lateral direction (‘unzip’ the fascia from the muscle). It should go easy, if not, you are likely injecting into the muscle. Advised is to inject small boluses of 5ml alternated with negative aspiration, to ensure proper spread. If necessary, reposition your needle so that anaesthetic spreads within the whole compartment. If the anaesthetic spreads above the fascia, or within the muscle, reposition. If there is noticeable resistance, reposition.
Withdraw the needle and dress the skin.
SUPRA-INGUINAL APPROACH
There are different ways to this, all with the same end point. The operator can start with a similar position as the above and move the probe cranially following the sartorius & iliopsoas muscle. The most used technique is however the following:
Place your in a sagittal plane, with the marker pointing cephalic, over the anterior superior iliac spine (ASIS). After moving is slightly medially, you will be able to identify the iliopsoas, running over the iliac brim, the internal oblique muscle cranially and the sartorius muscle caudally. The fascia of the latter two muscle forms a bright white shape called the ‘bowtie sign’, with superficial the deep circumflex artery.
Insert the needle above the inguinal ligament and advance it beneath the fascia.
After a negative aspiration, inject 1-2ml to confirm the right position. The fascia should ‘unzip’ from the muscle, pushing the deep circumflex artery upwards. Again, if injection is difficult, you are likely in an incorrect position.
The local anaesthetic should spread cranially towards the abdominal muscle. A similar technique of negative aspiration and boluses can be used to ensure this.
Withdraw the needle and dress the skin.
Gallery.
Author: Ruth Sneep | Editor: Felipe Urriola
References.
The National Hip Fracture Database Report on 2021 (NHFD 2022 annual report). The Royal College of Physicians. National Falls and Fragility Fracture Audit Programme (FFFAP). Available at: https://www.nhfd.co.uk/2022report
Fascia iliaca compartment block for control of hip/femur fracture pain in adult patients, BestBETs. S Elkhodair, T Jaiganesh. Last updated 25th March 2010. Available at: https://bestbets.org/bets/bet.php?id=1024
Pedersen S, Borgbjerg F, Schousboe B, et al. A comprehensive hip fracture program reduces complication rates and mortality. J Am Geriatr Soc. 2008;56(10):1831-1838. https://www.ncbi.nlm.nih.gov/pubmed/19054201.
Beaudoin FL, et al. A comparison of ultrasound-guided three-in-one femoral nerve block versus parenteral opioids alone for analgesia in emergency department patients with hip fractures: a randomized controlled trial. Acad Emerg Med. 2013;20(6):584-91.
Newton-Brown E, et al. Audit improves emergency department triage, assessment, multi-modal analgesia and nerve block use in the management of pain in older people with neck of femur fracture. Australas Emerg Nurs J. 2014;17(4):176-83.
Fascia Iliaca Block in the Emergency Department. The Royal College of Emergency Medicine. Best Practice Guideline. Published May 2020. Available at RCEM.co.uk.
Dolan J, Williams A, Murney E, Smith M, Kenny GNC. Ultrasound guided fascia iliaca block: a comparison with the loss of resistance technique. Reg Anesth Pain Med 2008; 33: 526e3.
Desmet M, Vermeylen K, Van Herreweghe I et al. A longitudinal supra-inguinal fascia iliaca compartment block reduces morphine consumption after total hip arthroplasty. Reg Anesth Pain Med 2017; 42: 327e33.
Kumar K, Pandey RK, Bhalla AP et al. Comparison of conventional infrainguinal versus modified proximal suprainguinal approach of Fascia Iliaca Compartment Block for postoperative analgesia in Total Hip Arthroplasty. A prospective randomized study. ACTA Anaesth Belg. 2015; 66 (3):95-100